A cyst is defined as “an epithelial lined pathologic cavity”. The periapical/radicular cyst is an odontogenic cyst. The classification of the cysts can be seen HERE. It is important to read for ADC Exams or NEET MDS purpose.
Periapical/Radicular cyst
Periapical cysts are inflammatory cysts. Their epithelial lining originates from the odontogenic epithelium of the tooth buds that remains within periodontal ligaments (epithelial rests of Malassez) after completion of tooth maturation. Due to inflammatory response, the epithelial rests of Malassez start proliferating and provide cystic lining.
Etiology and Pathogenesis of Periapical Cyst
Periapical/Radicular cyst develops from an already existing periapical granuloma located at the apex of a non vital tooth that has been rendered dead due to caries or trauma. Periapical granulomas are initiated and maintained by the toxins produced by the necrotic pulp tissues. When the epithelial rests of Malassez are stimulated by the inflammatory products of the pulp necrotic tissues, they proliferate and surround the granulation tissues.
Thus the epithelial lining of the cyst tries to separate the granulation tissue from the irritating toxins from the necrosed pulp. The breakdown of granulation tissues inside cyst increases the osmotic pressure and causes fluid ingress through cyst lining from the surrounding tissue, thus expanding the cyst size by osteoclastic activity at the periphery. Other bone resorbing factors like prostaglandins, interleukins, proteinases from inflammatory cells and cells in peripheral area of the lesion also help in cyst enlargement.
Clinical Features
Periapical cyst constitutes 50% to 75% of all cysts found in the jaws. They are mostly found in the third to 6th decades of life. They are mostly located in the anterior part of maxilla, followed by posterior part of maxilla, posterior mandible and finally followed by anterior part of mandible.
They are asymptomatic and are found by chance on radiographs during routine radiographic examination. They cause bone resorption but do not cause bone expansion. By definition, presence of a nonvital tooth is necessary for the diagnosis of periapical cyst.
On radiograph, they are round to ovoid in shape and normally less than 1.5mm in size, although the size may range from a few millimetres to several centimetres. They are usually surrounded by a radiopaque thin margin which is contiguous with the lamina dura of the involved tooth, that may be absent in a fast growing periapical cyst. Root resorption of the involved and neighbouring tooth may be present in a long standing cyst.
 |
| [1] |
Histopathology
Periapical cyst is lined by nonkeratinized stratified squamous epithelium. It is usually infiltrated with a large number of neutrophils and few lymphocytes. In connective tissues, plasma cells along with mixed inflammatory cells are in abundance. Russell bodies are spherical, refractile, gamma globulin of varying size packed into the plasma cell’s cytoplasm and push the nucleus to the edge of the cell, and are found in the peripheral areas of the cyst.
In a few instances of periapical and dentigerous cyst, hyaline bodies within the epithelium are found and are known as Rushton bodies. They have pinhead or curve shape, concentric lamination and occasional basophilic mineralisation. They are supposed to originate from previous haemorrhage and are of no clinical significance.
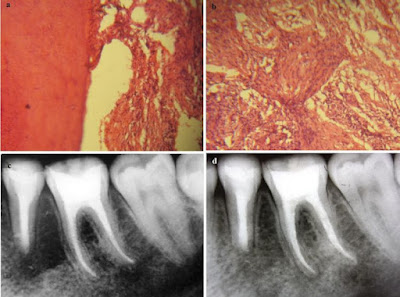 |
| (a, b) Histological examination of the cyst (magnification 40 X); (c) Radiograph taken six months after surgery; (d) Radiograph taken three years after surgery.[2] |
Treatment of Periapical Cyst
The non vital tooth associated with cyst should be removed. The other conservative treatment is endodontic therapy of the involved tooth along with apicoectomy and curettage of the cystic lining. Recently, they are being treated by only RCT as most of the periapical radiolucency in periapical granuloma. If the radiolucency does not regress or any symptom develops, the tooth should be removed and the cystic lining should be removed by curettage.
Ref:
- https://www.abstractsonline.com/EPosterViewer/DisplayImage.aspx?mKey={22FDF1E0-BB98-47D9-B084-94213A1B7D4D}&cKey={126B55E6-0AEE-48C3-B751-F1B1ADD15740}&RefID=2881
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3782982/figure/F2/