|
| Permlastic is a polysulfide, condensation-cured, elastomeric impression material in three viscosities |
A coaching institution for ADC examination, ORE and Government dental job exams.
Polysulfide Impression Materials
Non-carious loss of tooth structure
Types, clinical features, Causes prevention & treatment
Types of tooth wear
- Abrasion
- Attrition
- Erosion
- Demastication
- Abfraction
NEET 2022-23 Exam Dates Declared by NBE for NEET-MDS UG and PG
- NEET-MDS 2023: January 8, 2023
- DNB/DrNB Final Practical Examination – June 2022: October/November 2022
- Foreign Medical Graduate Examination (FMGE) December 2022, Foreign Dental Screening Test (FDST) 2022: December 4, 2022
- Formative Assessment Test (FAT) 2022: December 10, 2022
- DNB/DrNB Final Theory Examination – December 2022: December 21, 22, 23 and 24, 2022
- Fellowship Entrance Test (FET) 2022: January 20, 2023
- FNB Exit Examination 2022: February/March 2023
- DNB/DrNB Final Practical Examination – December 2022: Feb/March/April 2023
- NEET-PG 2023: March 5, 2023
 |
| Distribution of subject wise questions in NEET MDS examination. |
Harmful Effects of Excessive Radiation
The harmful effects of the excessive dose of the ionizing radiation can be divided into two types. These are as follows:
- Deterministic effects and
- Stochastic effects
We shall discuss them one by one in detail.
Radiography: Radiation Safety
In earlier articles on radiography, you studied the effects of ionizing radiation on biological tissues. These effects can be divided into two types- Deterministic and Stochastic. Therefore, the radiation safety becomes of paramount importance white taking a radiograph.
Radiography: Radiation Physics
In this article termed as radiation physics, we shall talk about the ways, the x-rays are produced, the events that occur at atomic level during their production and how can one save oneself and others.
Production of X Rays
Electrons that travel from the filament to the tungsten convert part of their kinetic energy into x-ray photons. This phenomenon occurs by the formation of bremsstrahlung and characteristic radiation.
Radiography: Radiation Biology
Radiation Biology
Radiation biology is the study of effects of ionizing radiation on living systems. In this article we shall talk about the harmful effects of ionizing radiation on tissues, how does it occur, and how sensitive different types of cells are?
The effects of radiation on the tissues can be divided into 2 broad categories. The Deterministic and Stochastic effects.
Cysts of the Jaws and Neck: Classification
Cysts of the Jaws and Neck
Odontogenic Cysts
- Periapical (Radicular) Cyst
- Lateral Periodontal Cyst
- Gingival Cyst of the Newborn
- Dentigerous Cyst
- Eruption Cyst
- Glandular Odontogenic Cyst
- Odontogenic Keratocyst
- Calcifying Odontogenic Cyst
Nonodontogenic Cysts
- Globulomaxillary Lesion
- Nasolabial Cyst
- Median Mandibular Cyst
- Nasopalatine Canal Cyst
Pseudocysts
- Aneurysmal Bone Cyst
- Traumatic (Simple) Bone Cyst
- Static Bone Cyst (Stafne’s Bone Defect)
- Focal Osteoporotic Bone Marrow Defect
- Soft Tissue Cysts of the Neck
- Branchial Cyst/ Cervical Lymphoepithelial Cyst
Periapical/Radicular Cyst
A cyst is defined as “an epithelial lined pathologic cavity”. The periapical/radicular cyst is an odontogenic cyst. The classification of the cysts can be seen HERE. It is important to read for ADC Exams or NEET MDS purpose.
Periapical/Radicular cyst
Periapical cysts are inflammatory cysts. Their epithelial lining originates from the odontogenic epithelium of the tooth buds that remains within periodontal ligaments (epithelial rests of Malassez) after completion of tooth maturation. Due to inflammatory response, the epithelial rests of Malassez start proliferating and provide cystic lining.
Dentigerous/Follicular Cysts
Dentigerous (Follicular) Cysts are the second most commonly occurring odontogenic cysts after periapical cyst and the most common developmental cysts of the jaws. By definition, a dentigerous cyst is attached to the tooth cervix (enamel-cementum junction) and encloses the crown of the unerupted tooth.
 |
| Photograph1: Dentigerous cyst surrounding the crown of right mandibular third molar and going upward in ascending ramus. [1] |
Etiology and Pathogenesis of Dentigerous Cyst
A dentigerous cyst originates from the enamel organ remnant or reduced enamel epithelium. The expansion of the dentigerous cyst is related to epithelial proliferation, release of bone-resorbing factors, and an increase in cyst fluid osmolality.
Clinical Features of Dentigerous Cyst
Dentigerous cysts are most commonly seen associated with third molars and maxillary Canines. The peak incidence of dentigerous cysts occurs between twenty to 40 years. Males have more predilection with a ratio of l.6 to 1.
Dentigerous cysts are generally symptomless. The delayed eruption is the most common indication of dentigerous cyst formation. This cyst can achieve significant size, occasionally causes cortical bone expansion but rarely reaches a size that predisposes the patient to a pathologic fracture.
Radiographically, a dentigerous cyst manifests as a well-defined, unilocular or sometimes multilocular radiolucency with corticated margins in attached with the crown of an unerupted tooth. The concerned unerupted tooth is mostly displaced. In the mandible the related radiolucency may extend superiorly from the third molar site into the ramus or anteriorly and inferiorly along the body of the mandible. In maxillary dentigerous cysts in the canine region, extension into the maxillary sinus or to the orbital floor may be seen.
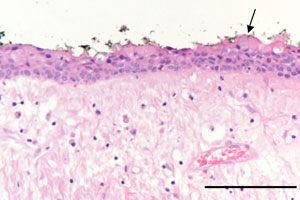
Histopathology.
The cyst is lined by stratified squamous epithelium. In a noninflamed dentigerous cyst the epithelial lining is nonkeratinized. It remains approximately four to six cell layers thick. Sometimes, numerous mucous cells, ciliated cells, and rarely, sebaceous cells may be found in the lining of the epithelium. The epithelium-connective tissue junction is generally flat. But when secondary inflammation established, epithelial hyperplasia may be noted.
Differential diagnosis
When it is small, it is difficult to differentiate a dentigerous cyst from a large but normal dental follicle. When larger, the differential is essential that of lytic lesions of the jaw and includes:
- periapical cyst
- aneurysmal bone cyst
- ameloblastoma
- odontogenic keratocyst
- fibrous dysplasia
- Stafne cyst
Treatment
Removal of the associated tooth and enucleation of the soft tissue part is definitive therapy in most cases. When cysts affect significant portions of the mandible, exteriorization or marsupialization of the cyst is done to allow for decompression and subsequent shrinkage of the lesion followed by surgical enucleation.
Ref: